Client Context
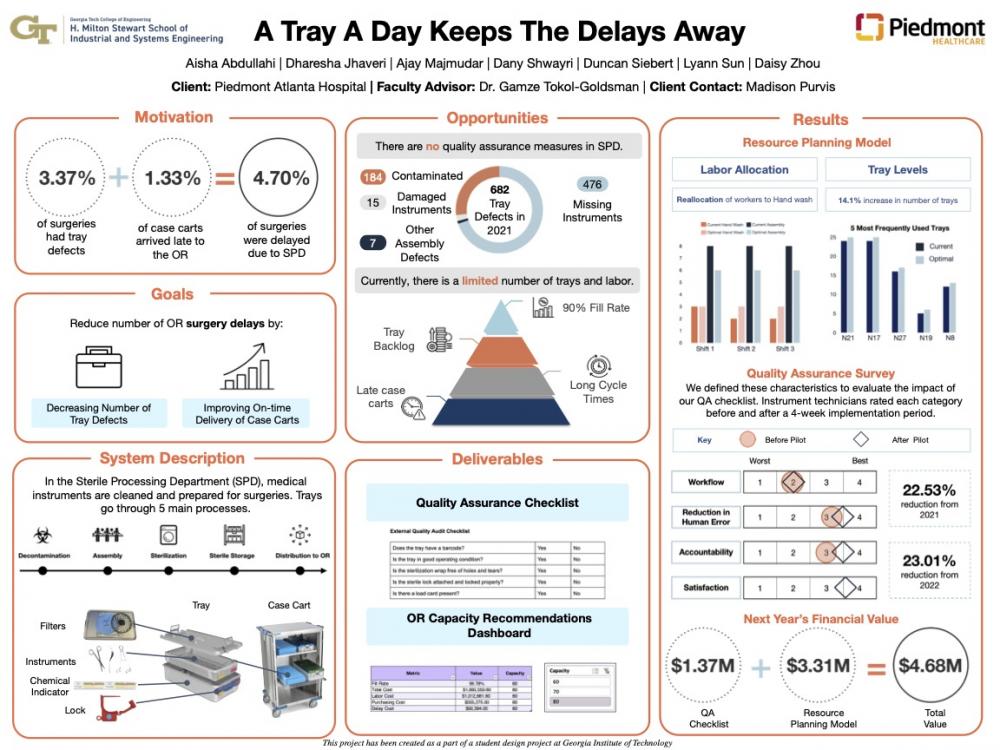
The client, Piedmont Atlanta Hospital (PAH), is a 643-bed, private, not-for-profit hospital serving the metro Atlanta community. The team worked with the Sterile Processing Department (SPD), which is the department that cleans, packages, and sterilizes trays containing instruments after they were used in surgeries. SPD processes around 2,911 trays every week and can be split into 5 major functions: Decontamination, Assembly, Sterilization, Sterile Storage, and Distribution to the OR.
Project Objective
The goal was to reduce surgery delays due to SPD. In 2021, 4.7% of surgeries were delayed due to SPD while the average delay time for first surgeries of the day was 22.1 minutes. 3.37% of all SPD delays were due to tray defects, and 1.33% of them were due to a case cart (which are composed of trays) not arriving to the Operating Room (OR) on time. A tray defect is a tray that cannot be used in the OR due to human error when assembling a tray in SPD while on-time case cart delivery is affected by tray unavailability. With regards to on-time delivery, the team found that the root cause of these categories of delays was limited resources of SPD labor and trays.
Design Strategy
The team's first objective was to reduce the total number of tray defects caused at or before the Assembly Station to reduce the number of surgery delays. Since there were no quality assurance measures in place, the team implemented a quality assurance checklist at the end of the Assembly station to prevent defective trays from reaching the OR. When designing the checklist, the team shadowed instrument technicians to understand where the main pain points for human error were in the system and validated these sources of error with the supervisors. The second objective was to ensure an on-time delivery of case carts to the OR. From analyzing the system, the team utilized a metric called fill rate which was defined as the percentage of surgery demand met by immediate tray availability for on-time surgery starts. The team then narrowed the scope to focus only on the neurosurgery service line and created a simulation model using Simio to determine the optimal number of instrument technicians at Decontamination and Assembly per shift and the number of neurosurgery trays that achieve a minimum 95% fill rate for 3 OR capacity levels. The model was validated by running two bi-monthly periods which had the highest and lowest fill rates in 2021 and ensuring that the true values of fill rate and number of delays fell within the 95% confidence intervals of the model's results.
Deliverables
The team had 2 deliverables: (1) Quality Assurance Checklist and (2) Resource Planning Excel Dashboard. The checklist is paper-based, and the process includes 5 random checks per shift or 15 checks per day fortrays. The checklist is divided into internal and external quality assurance segments, and each question on the checklist addresses a certain type of tray defect. The Excel dashboard was created to provide the client the recommended labor and neuro-tray levels depending on the hospital's OR capacity level as well as the corresponding fill rate, labor cost, delay cost and purchasing cost. Based on the team's findings, there should be a reallocation of labor from Assembly to Decontamination with a 14.1%, 28.1%, and 28.7% increase in the top 50 most used neuro trays for 60%, 70%, and 80% OR capacity levels, respectively.