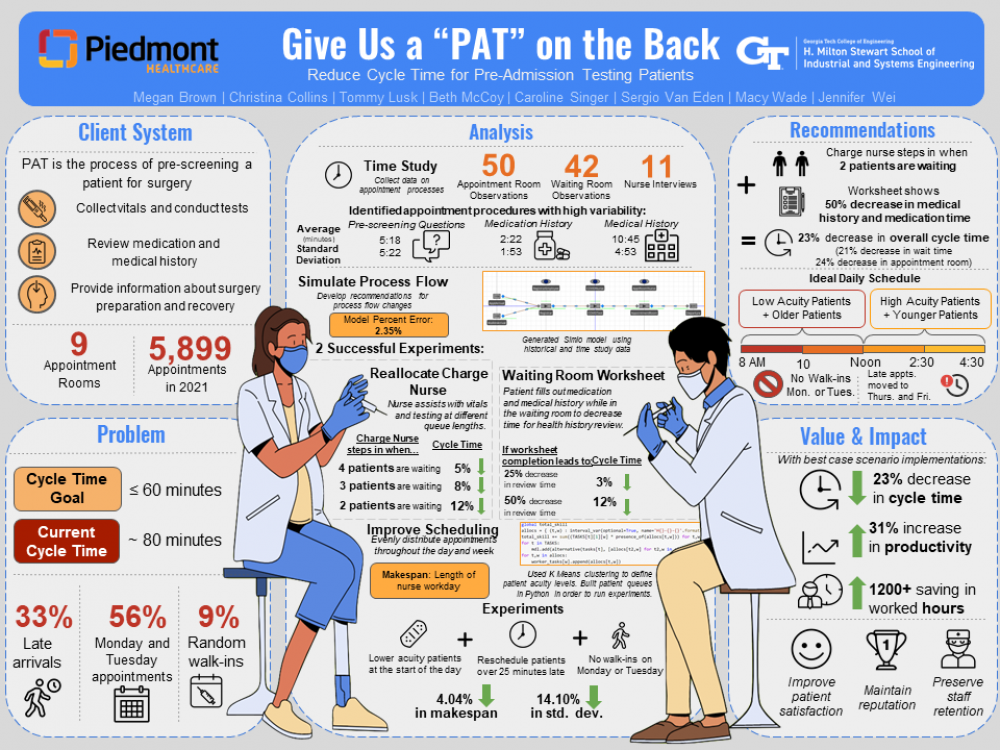
Client Context
As a leader in premium patient care, Piedmont Atlanta Hospital is visited by thousands of patients each year for surgical operations. Within the hospital, the Pre-Admission Testing (PAT) process is a critical step in a surgical procedure for the medical care team to gather essential patient information and assess a patient's readiness for surgery 1 to 30 days before their surgery date. In a typical PAT assessment, a PAT nurse will collect vitals, conduct medical tests, review the patient's health condition and medication history, and provide information regarding the patient's day of surgery. PAT operates from 8:00 AM to 5:00 PM, Monday - Friday. There are 9 appointment rooms in the department, and the number of nurses seeing patients each day can vary from 5 to 9 with an average 6.
Project Objective
Piedmont's PAT target service level is for average patient cycle time to be less than or equal to 60 minutes. Currently, around 67% of cases are over 60 minutes, and patient cycle times average 80 minutes and range from 8 to 297 minutes. Hence, this project's overall goal is to minimize patient cycle time. Key factors that contribute to long and variable cycle times are as follows: variable tests per patient health conditions and surgery type, lack of patient preparation for PAT, no policies in place for late arrivals and walk-ins, and clustered appointment distribution in the beginning of the week. Based on nurse interviews, surveys of surgeons' offices, scientific literature reviews, and on-site observations, there is an opportunity to streamline the PAT operational process flow by decreasing non-value added time to reduce overall cycle time. There is also an opportunity to provide scheduling recommendations that will reduce variability in the system.
Design Strategy
Process Flow Changes: The team initially constructed a baseline Simio model using historical data from the client and then extended the model to incorporate each step within the appointment room based on 50+ hours of shadowing appointments. The model has been set up to include 2 kinds of entity types (scheduled vs. walk-ins). The simulation acts as a diagnostic tool and allows for recommendations to be piloted before undergoing any larger investments. Multiple Simio experiments of different workflow designs were performed to find the design with the largest cycle time reduction. Scheduling Guidelines: Based on historical data, the team created 2 queuing systems that would simulate patients going through PAT in different orders. The first queue would take the patients in their originally scheduled order, run them through PAT, and see the amount of time it takes nurses to tend to all of those patients. The next queue would take the same exact patients and run them through PAT with the scheduling guidelines reordering and rescheduling patients more optimally throughout the week. Since acuity scores were not included in the original dataset, an acuity scale was created to use in the scheduling guidelines. For each type of surgery performed at Piedmont, an average operating time was found. A K-Means clustering algorithm was then used to cluster the surgery types into 5 categories (1 being lowest acuity, 5 being highest acuity) by minimizing within-cluster variances. After defining patient acuity, various experiments were run on these historical queues to identify the scheduling arrangements with the most impactful standard deviation and makespan reductions, where makespan is the time between the start of the first appointment and the end of the last appointment of the day. Decreasing the makespan will decrease that workday for nurses and increase their productivity, while decreasing the standard deviation of the workday length each day will help to stabilize the PAT system.
Deliverables
Recommended Process Flow Changes: The 2 most successful Simio experiments consist of reallocating the charge nurse and implementing a patient worksheet in the waiting room. The charge nurse is responsible for directing logistics within the department and is trained to be patient-facing, meaning that they can step in to assist with collecting vitals and conducting medical tests for patients in between duties when PAT gets extremely busy. The reallocating the charge nurse experiment entails that once a specific number of patients are in the queue leading into the appointment room, the charge nurse would step in to help with testing when they are available. The largest cycle time reduction of 12% occurs when the nurse steps in when 2 patients are waiting. The results of this experiment could also be applied to the addition of another nurse or medical assistant to the system that performs those same tasks while patients wait. In the patient worksheet experiment, patients would complete a worksheet in the waiting room that covers information in the medication and medical history review in order for the nurse to spend less time during this step later on in the appointment room. Scientific research has shown that patients sense that they are being "moved" through the process if they are given opportunities and activities to productively "fill up" their wait time. As observed in time studies, patients who had their medication and medical history prepared on a piece of paper prior to their PAT appointment could allow the nurses to spend less time inquiring patients about their health conditions and simply read the paper and quickly type the information onto the computer. The largest cycle time decrease of 12% happens if there is a 50% decrease in the time for this health history review in real life. If both the charge nurse and patient worksheet redesigns were to to be implemented at their best case meaning a floating nurse steps in with testing when there are 2 people in the queue and that a patient worksheet would result in a 50% decrease in patient medication and medical history review in the appointment room, the overall cycle time would be reduced by 23% down to 62 minutes, which is close to the 60 minutes target. A pilot would be needed to assess the success of the changes through nurse feedback and cycle time data analysis if the department were to implement these redesigns. Recommended Scheduling Guidelines: Experiment results show that by having lower acuity and older patients in the morning and higher acuity and younger patients in the afternoon, a late policy that reschedules patients' appointments when they are more than 25 minutes late, and prohibiting walk-ins on Monday or Tuesday, the makespan and standard deviation are reduced by 4% and 14%, respectively. If PAT were to implement these scheduling policies, the department would see a more consistent number of patients coming to PAT each day and shave a few minutes off of the workday. This aids in preventing nurse burnout and easing the piled up workload in the beginning of the week. There will always be exceptions to these proposed policies with out-of-state patients, traffic, and PAT being required before an imminent surgery. Having these policies in place, however, can encourage patients to arrive early and come later in the week when they make their PAT appointment.