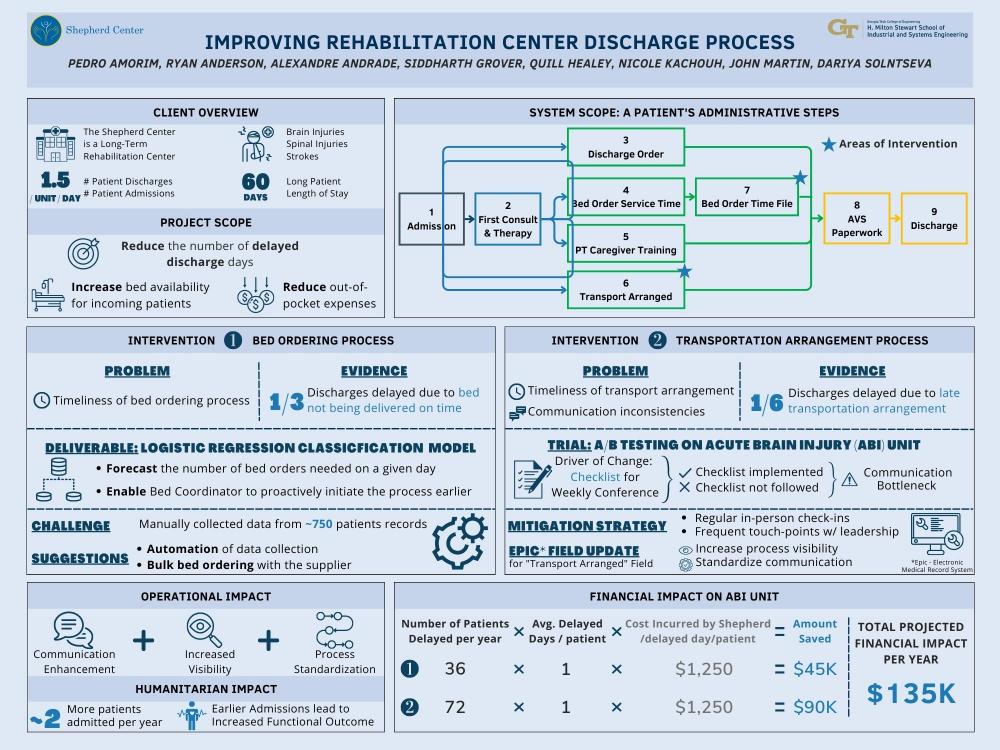
Client Context
The Shepherd center is a private, non-profit neurorehabilitation facility, located in Atlanta, Georgia. Shepherd specializes in rehabilitation programs that focus on helping people with severe brain and spinal cord injuries achieve the highest possible level of independence and quality of life.
Project Objective
Our primary objective is to reduce the number of delayed discharge days, which refer to the days that a patient remains at the Shepherd Center after their official discharge date due to non-medical reasons. Specifically, we are looking into delayed discharge days caused by two administrative processes:
-
Bed related delayed discharge days – when a hospital bed required by a patient at their home has not been delivered.
-
Transportation related discharge days – when transportation required to take a patient from Shepherd to their next location has not been arranged to pick them up on day of discharge.
Design Strategy
Bed and Transportation delayed discharge dates are not covered by the patient’s insurance and result in a daily cost of $1,250 to Shepherd. Additionally, early initiation of the rehabilitation process for neurologically injured patients has been scientifically proven to be strongly correlated with better functional outcomes, which is directly related to Shepherd’s mission.
For the bed-related delayed discharge days, it was discovered that the step in which the patient’s need for a bed is identified is the primary cause of delays. To address this inefficiency, we propose to give the stakeholder responsible for the bed ordering process more autonomy. This solution is driven by a classification model which, based on a series of characteristics, assigns a probability of needing a bed to each patient, allowing the DME coordinator to estimate the number of beds needed on any given day.
For the transportation-related discharge days, both the transportation arrangement timeline and communication between the stakeholders are identified as primary causes of delays. Our proposed solution involves incentivizing stakeholders to initiate the entire process earlier as well as transforming already existing communication channels into a standardized mode of communication. To validate these solutions, we conducted a trial in one of the units at Shepherd. The changes were driven by updates to an already existing checklist that was used during the weekly team conference to guide discussions and prompt stakeholders to act effectively and in a timely fashion on each patient’s case.
Deliverables
Along with the manually collected dataset, logistic regression model, GUI, and checklist, we are also delivering a Power Bi dashboard to democratize stakeholder visibility.
Value and Impact
Given that the shifted bed ordering process timeline driven by the logistic regression model eliminates all bed related discharge days, Shepherd’s ABI unit will save $90,000 per year. Likewise, given that our shifted transportation arrangement timeline and redefined communication channels eliminate all transportation related discharge days, Shepherd’s ABI unit will save $45,000 per year. Along with these monetary benefits, our changes will also allow Shepherd to see more patients and treat incoming patients earlier. Finally, these changes will help Shepherd uphold its reputation with its partners – the center has historically lost transportation partners as result of requesting transportation for a patient from them the day of or prior to this patient’s discharge.