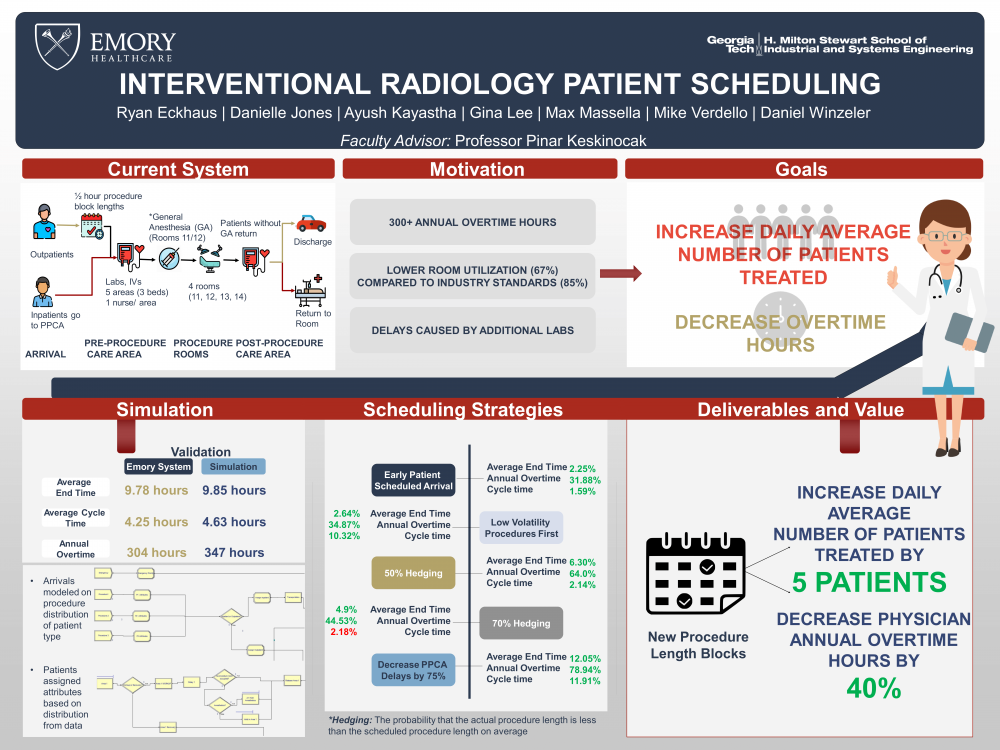
Client Context
Emory University Hospital at Clifton IR Department, located in Atlanta, Georgia, performs around 5,400 procedures annually. With the rising demand for minimally invasive surgeries, EUH Clifton IR has a goal to increase the number of procedures (currently 18) completed over a 10 hour workday (7:30 am - 5:30 pm) with their current available resources.
Project Objective
Currently, the clinic schedules outpatients based on primary care physicians’ referral, physician availability, patient location, and patient preference. When the scheduler receives a surgery order, they refer to a table that outlines procedure lengths in 30 minute blocks. This causes EUH Clifton IR to experience inconsistent levels of hedging in their scheduling. Hedging measures the probability that the actual procedure length is less than the scheduled procedure length on average.
As a result of our observations and interviews with our client, our team narrowed down our focus to the scheduling of procedures. Under this process, there are a number of delays within the system because of inconsistent and inefficient scheduling. While developing our solution, our client asked that we make sure to help them maintain the same level of care as well as not increase the current number of overtime hours for their employees.
Design Strategy
After seeing that multiple procedures rooms were idle for lengthy periods of time and the lack of scheduling consistency, our team decided to build a simulation model to help evaluate the effects of certain changes to the system.
The proposed solution involves reducing controllable delays within the system as well as readjusting the scheduling time blocks to align with the distributions of procedure lengths. The team grouped the procedures into 15 groups by mean, standard deviation, and whether or not anesthesia is required. The frequency of each group was used to calculate an average daily arrival rate for the group. Groups are assigned to patients as an attribute in the simulation.
To validate the simulation with the current EUH system, our team ran the simulation using inputs from the hospital’s current schedule. ur team ran the simulation for 100 replications and based the validation on three metrics: average end time of the day, average patient cycle time, and annual overtime hours. From our validation we found that there was no significant difference between the simulated and actual average end time and cycle time distributions.
Deliverables
For our client, we ranked the changes in order of ease of implementation and positive impact: 50% hedge scheduling, Change pre procedure requirements, Earlier patient scheduled arrival, 70% hedge scheduling, Low volatility procedures first. We also provide a table of procedures with the average procedure lengths for out client to help them better align their scheduling to the actual length of the procedures and decrease delays.