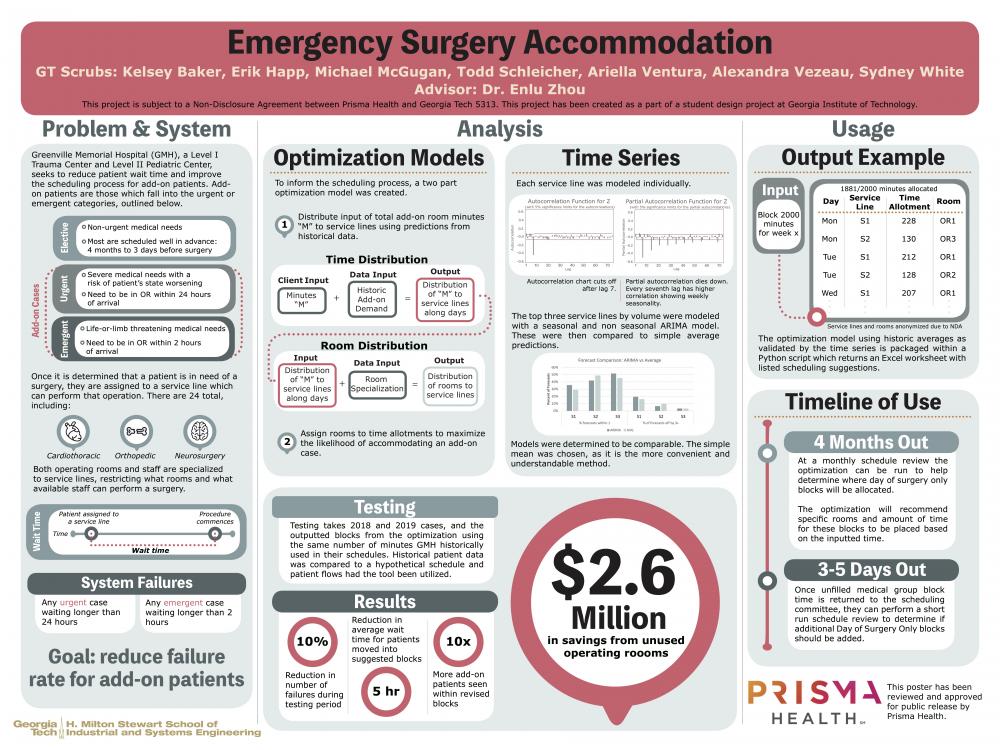
Client Context
Prisma Health’s Greenville Memorial Hospital is a Level I Trauma Center located in Greenville, South Carolina. As a Trauma Center, the hospital provides 24-hour services and reserves at least one operating room for an emergency arrival at all times. The hospital has 33 operating rooms which are used to service patients both scheduled in advance (“elective” cases) and in immediate need (“add-on” cases). Four months in advance, a scheduling committee at the hospital allots blocks of time in rooms to medical groups, reserving unassigned time in rooms as either “first-come first-served” (FCFS) or “day of surgery only” (DoSO) blocks. Medical groups can then schedule elective surgeries during their allotted blocks. Medical groups not allotted blocks are allowed to schedule cases in FCFS rooms once the block schedule is released, and these rooms are filled months in advance. DoSO blocks exist to serve add-on cases, yet these blocks do not efficiently serve add-on cases.
Project Objective
The goal of this project is to improve the system’s performance in accommodating add-on cases. Relevant success metrics include reducing add-on wait times, utilization of DoSO blocks, and the reduction of system failures. A failure is either an emergent case which waits over 2 hours for an operation or an urgent case which waits over 24 hours for an operation. Currently, add-on cases have failure rates higher than 10%. Analysis also indicates that DoSO blocks are underutilized. Only 15% of the minutes distributed to DoSO blocks are utilized for add-on cases. The project aims to reduce the wait time of add-on patients and decrease system failures by reallocating the DoSO blocks to better address variable add-on patient demand within all service lines.
Design Strategy
The team approached the problem by first analyzing historic data and finding trends to determine points of opportunity for improvement. The historical data set indicated that the system’s arrival process is seasonal by days of the week. It became clear that the rooms and days of the week in which DoSO blocks were being scheduled were incongruent with this variable daily arrival process. The team hypothesized that the strategic redistribution of DoSO time would improve the system’s overall performance in accommodating add-on patient operations. To test our hypothesis we created an optimization model which reallocates DoSO minutes to rooms along days of the week which reflect historic add-on arrivals by each service line.
We tested our methodology by examining add-on cases from January 2018 through June 2019 and evaluating the benefits of our model’s proposed DoSO blocks. For each week in the test period, add-on cases for that week were evaluated to see if they would benefit from being seen in a proposed DoSO block. For example, consider an urgent general surgery case that came in on a Monday morning and was seen Tuesday morning. The testing methodology would see if this case could be seen in the proposed Monday general surgery DoSO block. So long as the expected duration of the surgery can fit in the time remaining in the block, the test would record the case as accommodated in the block and retroactively calculate its new wait time.
Deliverables
Deliverables include:
- An executable program which runs the optimization tool
- The program allows the client to input any value representing the number of minutes desired for DoSO blocks within a business week. It then produces an Excel spreadsheet with all recommended allotments, including operating room, block duration, and day of the week.
- Manual describing how to use this program in a meaningful way
- The manual describes the functionality of the tool and explains its main objectives. The client has expressed interest in continuing to experiment with the tool, so this will be helpful in familiarizing hospital officials with its inner workings.
- Additional files with meaningful analytical insights
- The scheduling committee is just beginning to use data in its decision-making process. Therefore, committee staff can use statistics derived from analysis within these files, particularly those concerning room utilization, service line operation duration, and add-on and elective demand.
- Time series analysis
- Time series description will help the perioperative staff at GMH understand the results of our time series, should they choose to investigate this model further.
- Supplemental Python scripts for cleaning and testing
- As the hospital gathers more data, the parameters input to the optimization tool must be updated accordingly. Therefore, scripts which clean the input data (primarily data associated with demand) and test the new results are critical for the continued relevance of the optimization tool.
Recommendations:
When planning for the use of DoSO blocks, it is necessary to strictly prioritize emergent cases over urgent cases, and urgent cases over electives. If the hospital chooses to schedule a DoSO block, the team recommends placing it towards the end of the day. This way, urgent case demand (which represents a significantly higher volume than emergent cases) can accrue throughout the day and be served towards the day’s end. Surgeries should still be scheduled on a priority basis with the most time-sensitive cases scheduled sooner.
For the prediction of add-on case arrivals, a table describing the average number of add-on cases for each service line is included in Appendix C3. When the Block Scheduling Committee takes release time from a medical group, it should consult the chart of averages to understand the possible number of add-on case arrivals before allocating the time to FCFS blocks. If there is an insufficient number of DoSO blocks during a day, the hospital should use this released time towards DoSO blocks.
Finally, the optimization tool is versatile in its ability to recommend DoSO blocks given any user input. Hospital officials will benefit through the trial of its recommendations using different values of M, as the realized changes may offer great opportunities for system improvement. While no policy may offer perfect circumstances for a system with variable parameters, inclusion of the tool in scheduling practices can introduce significant enhancements to the long-term GMH patient experience.