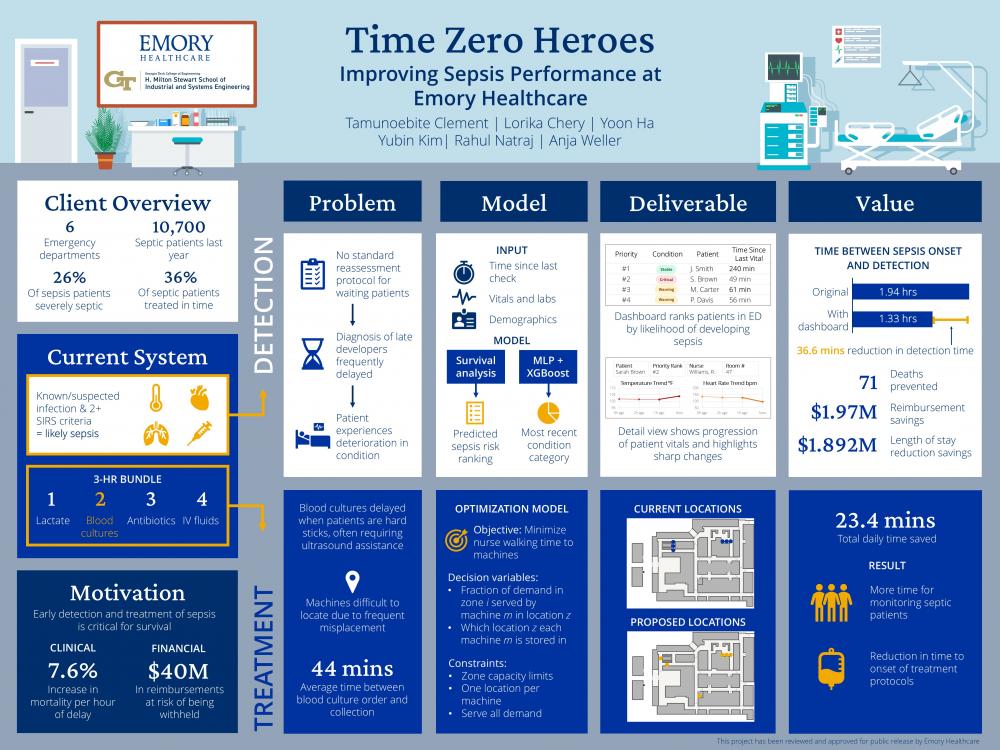
Client Context
Emory Healthcare is the largest healthcare provider in Georgia, operating six metro-Atlanta hospitals. Their emergency departments serve as the first point of care for many patients who progress to sepsis. Sepsis is a life-threatening condition caused by a dysregulated host response to infection that can progress to septic shock, which correlates to profound circulatory, cellular, and metabolic abnormalities and a greater risk of mortality if untreated.
Project Objective
Emory's emergency departments face significant challenges in the timely identification and treatment of sepsis. Inconsistent reassessment in the waiting room causes developing sepsis symptoms to go undetected until deterioration is obvious. Once sepsis is recognized, treatment delays continue because blood culture collection, a key step in the sepsis treatment bundle, often depends on locating ultrasound machines that are stored unpredictably across the ED. These delays put patients at risk and threaten Emory’s ability to meet the SEP-1 compliance threshold mandated by the Centers for Medicare and Medicaid, which affects the hospitals' reimbursements.
Design Strategy
Diagnosis
To address delays in diagnosis, our strategy centered around the goal of creating an assistive tool for nurses to track patients at risk of sepsis effectively. We approached this by combining two analytical methods: a survival analysis model for predicting individual risk progression and an ensemble machine learning model for condition classification. The survival analysis model was created using the Cox Proportional Hazards Model, based on its reliability in healthcare risk prediction. This model answers the question: “Who should I see next?” Patients who are both at higher risk and have not been reassessed recently will rank higher on the list. For the ensemble machine learning model, we combined an XGBoost and a neural network to leverage the unique strengths of each model structure. This status validates the priority ranking by indicating how critically ill the patient is based on the last vital check, helping nurses understand why a particular patient needs immediate attention.
Treatment
Delays in treatment were noted to cause operational setbacks that led to timing failures for critical interventions, hence causing the SEP-1 compliance rate to decline. Blood culture collection served as the most consistent bottleneck, especially as many sepsis patients fall under the “hard-stick” umbrella, meaning that they require ultrasound guided access for a blood draw. After observations at the Emory University Hospital Midtown location, it was noted that these ultrasound machines were inconsistently stored and difficult to locate, creating an average 44-minute delay before cultures could be drawn, and initial interventions could begin. To address this, we developed an optimized placement strategy that aligns machine availability with zone-level demand and reduces avoidable walking time. This configuration improves access to ultrasound-guided draws and supports the timely initiation of both the 3- and 6-hour SEP-1 bundles.
Deliverables
Our first deliverable to address delays in diagnosis is a patient priority dashboard that helps nurses identify which patients need reassessment most urgently. The user interface of the dashboard was developed using TypeScript. From the main page, nurses see a patient list that is ranked based on our survival analysis model. When the ED is busy, nurses can efficiently find specific patients with the search bar at the top. Patients can also be filtered by their primary nurse, allowing nurses to focus only on their assigned patients. If nurses click on a patient’s entry, they are directed to the condition status page, which is designed to provide a clinical snapshot of the patient’s condition, including vital trend graphs, patient info, and active comorbidities. If there is a rapid change in the patient’s vital signs, the trend graph is highlighted to instantly draw the nurses’ attention.
Our second deliverable is a recommendation for an optimized allocation strategy for the ultrasound machines within the Emory Midtown Emergency Department, developed in Python. We also recommend that Emory expand existing machine tracking capabilities beyond the charge nurse of the facility, along with centralizing machine error reporting consolidating downtime tracking.
Value and Impact
Together, these tools give nurses a clearer sense of who needs attention and remove avoidable delays when treatment begins. Implementation of our improvements would yield a 36.6-minute reduction in sepsis diagnosis time, preventing an estimated 166 cases of severe sepsis and 71 deaths annually. These figures are based on backtesting using historical data to simulate nurses checking patients based on our dashboard. Additionally, improvements in ultrasound machine placement would yield 142 hours in retrieval time saved annually for nurse staff. The total impact of our deliverables includes $3.86 million in annual savings through improved SEP-1 compliance and reduced length of stay, demonstrating how addressing fundamental workflow inefficiencies can simultaneously improve patient outcomes and financial performance.